I want you to know your dedication, passion, and intelligence doesn’t go unnoticed. As a disabled young adult with complex conditions, I have had more interaction with you than my peers, my parents, and their parents. My life has been saved by you and your peers countless times and your knowledge, compassion, and care has given me the opportunity for a life outside of the hospital. For that and many other reasons I am grateful. In the many hours of I have spent interacting with all of you, I feel as though I get to know many of you well. From that, as well as my experience working in the medical field, I write to you this post in hopes that you hear me, the me that is uneffected by my social anxiety, acute medical condition, or time. I hope that some perspective is gained from this but at the very least I hope you read it and know that I am still here with the same appreciation for who you are and what you do.
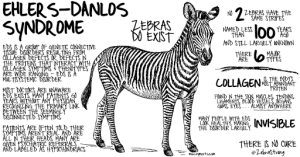
I have several complex medical conditions, many which lack education and understanding within the medical community and some which are vague/hidden enough that by their clinical presentation could be any number of things. I have issues that present “atypically” “weird” or “just don’t fit” with the models you were trained on. It is very annoying by the way. I have been misdiagnosed, mistreated, and misinterpreted more times than I can count. (For a great article on that, read this!) I am thankful that over time, more knowledge and direction has come my way and we now have a decent understanding of what is “wrong” with me (though of course there are still plenty of mysteries). Due to my experiences, I struggle in how to approach new providers. Yes, I have anxiety but this is more than that. Ultimately, with each new interaction the thought that runs through my head, and many of my chronically ill friend’s heads, is how do I need to act/present things to be taken seriously but not be flagged as crazy, too knowledgable (yes, unfortunately thats a thing), or disrespectful of the professionals knowledge/training. Interacting with you comes in two forms for me, voluntary or involuntary (emergency situations) but both come automatically come with the same calculations.
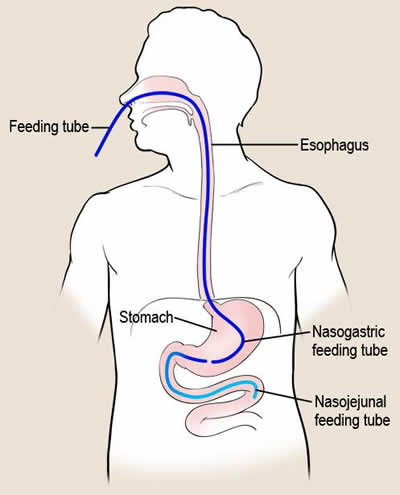
How do I explain that my dystonia might not look like primary dystonia, because it’s not, but is caused by mast cell activation in the brain possibly tied with my connective tissue disorder also maybe my autonomic dysfunction and we can’t really test any of those to confirm them but this is not a new problem and from many months of trial and error we have found that treating it with xyz is most effective even though that contradicts the treatment for primary dystonia but yes, I know this its just not primary dystonia and I can’t prove it and I can’t show it to you but I have world renowned specialists helping me navigate this impossible situation and I don’t want it to seem like I am trying to undermine your knowledge and experience as a doctor but also know that it is likely your training and experience didn’t cover this because the human body is so complex and more and more diseases and processes are being discovered every day so how on earth could we train humans to know all that and be able to draw upon it at a moments notice in order to treat a patient quickly, safely and effectively?
In my mind, I try to judge who is open to the fact that they can be a great doctor and not know everything and that, in cases where people have weird, rare, or complex issues, your knowledge base might not cover what is needed to help that person and that is okay. I try and judge who might see my medical knowledge from starting nursing school, working in the medical field in many settings, managing my conditions, and just an interest as something negative or as a red flag for attention seeking, faking, or crazy. I try and judge if they might be able to see me beyond what I look like in that moment. I try and judge who might be having a bad day so that I can modulate myself as much as possible to make that day less bad. I try and judge who might get my sarcastic, dark sense of humor and who I need to be literal with. I try and judge how you will react when you get a test result back that is normal, even though things are clearly not normal. I try and judge who is reading this and thinking man, she is super anxious (yes, yes I am) or man, which doctor screwed her over that gave her this chip on her shoulder. It may suprise you that who I am today and how I approach this has been shaped by hundreds of experiences — good and bad — over more than 10 years of being sick.
I want you to know that I understand what its like to be in a stressful job where there are patterns to patient behavior. There are frequent flyers, red flags, abusers of the system. I can’t imagine how hard it would be to, especially in a setting like a emergency department, parse out who the abusers are and who aren’t. I know, especially if you’ve read this far, you care about your patients and do not want to do harm. I know the pressure to make the right decision is high and that is really hard. I hope that by sharing some of the things I got through, often before I even see you, it may help you understand patients like me.
-Your chronically ill patient